Bio-degradable cards
Every card imaginable!
|
Bio-degradable cards Every card imaginable! COPD Essentials Explained Causes Symptoms Treatment and Daily Life Management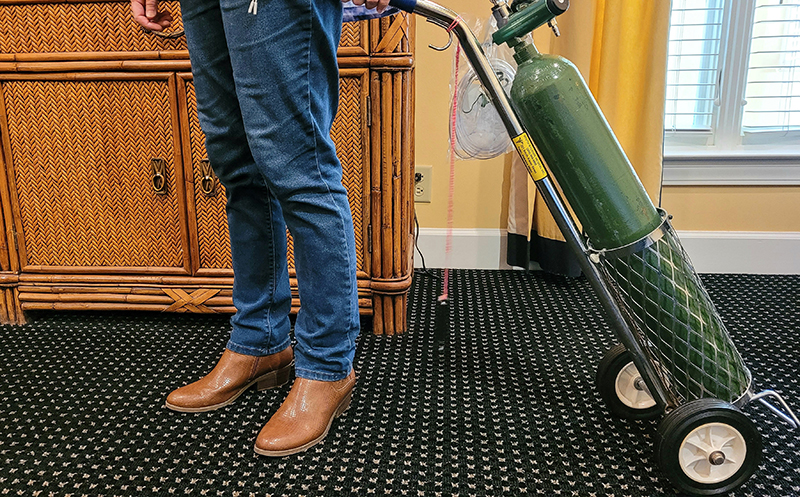
Table of ContentsIntroduction: Understanding COPD BasicsIf you're here reading this, chances are COPD has touched your life in some way—perhaps through a recent diagnosis for yourself or a loved one, or maybe you've noticed persistent breathlessness and want to learn more. It's completely normal to feel a mix of concern, confusion, or even frustration, but taking the time to understand the condition is a strong first step toward feeling more in control. In the UK as we approach 2026, chronic obstructive pulmonary disease (COPD) remains one of the most common long-term lung conditions. Recent estimates from Asthma + Lung UK and NHS data suggest around 1.7 million people are diagnosed, with likely many more undiagnosed. The numbers show how widespread it is, yet the encouraging side is that awareness and management options have improved greatly, helping many people live fuller lives despite the challenges. COPD isn't a single disease but an umbrella term for progressive lung conditions that make breathing harder over time. It involves damage to the airways and the tiny air sacs in the lungs, leading to narrowed passages, excess mucus, and reduced elasticity. This creates that familiar struggle for air, often accompanied by cough and fatigue. It's different from a short-term chest infection or asthma flare—COPD develops gradually and stays long-term, but it's not an inevitable sentence of constant decline. A helpful way to picture it is to think of healthy lungs as soft, expandable sponges that fill with air easily and squeeze it out without effort. In COPD, those sponges become scarred, stiff, and clogged, trapping stale air and making every breath require more work. Symptoms usually begin to appear after the age of 40, and the condition affects men and women in similar numbers these days. This guide is written with you in mind, drawing on trusted UK sources like the NHS, NICE guidelines, and Asthma + Lung UK to provide clear, up-to-date information as of late 2025. Whether you're looking for ways to spot early signs, understand treatments, or support someone close, the aim is to offer practical insights with empathy. Many people with COPD adapt successfully, finding new rhythms and enjoying what matters—let's walk through it together. 
Common Types of COPDCOPD doesn't look exactly the same for everyone; it includes a few main forms that can overlap, influencing how symptoms feel and how they're best handled. Recognising these can make a diagnosis feel less overwhelming and help tailor day-to-day strategies. While emphysema and chronic bronchitis are the two classic types, most people experience a blend of both (known as mixed COPD), and rarer variations like asthma overlap or genetic factors can also play a role. EmphysemaEmphysema mainly affects the tiny air sacs at the end of the airways—called alveoli—causing them to lose their elasticity, enlarge, and eventually break down over time. These sacs are crucial for transferring oxygen into the blood and removing carbon dioxide, so when they're damaged, air becomes trapped in the lungs. This creates a constant feeling of shortness of breath, even when you're not exerting yourself much. Common effects include:
It usually develops gradually from long-term exposure to irritants like cigarette smoke or pollution. The key point is that while the damage can't be reversed, stopping further irritation and using the right treatments can protect the healthy parts of your lungs and slow things down. Chronic BronchitisChronic bronchitis involves long-term inflammation and irritation in the larger airways (the bronchi), leading the lining to thicken and produce far more mucus than normal. This excess mucus clogs the airways, making it harder to breathe and harder for the lungs to clear themselves. Common effects include:
This type doesn't trap air in the same way emphysema does, but the constant inflammation and mucus make breathing feel laboured and increase infection risk. Treatments focus on reducing inflammation, thinning mucus, and helping you clear it more easily. Mixed COPDMost people diagnosed with COPD actually have features of both emphysema and chronic bronchitis—this is often just called mixed COPD and is by far the most common presentation. You might experience the trapped-air breathlessness of emphysema alongside the productive cough and mucus of chronic bronchitis, leading to a combination of symptoms that can feel more challenging day-to-day. Because it's so common, standard COPD management plans (inhalers, pulmonary rehab, etc.) are designed to help with both aspects at once, often bringing noticeable improvements in energy and comfort. Asthma-COPD Overlap Syndrome (ACOS)Some people have a blend of COPD and asthma features, known as asthma-COPD overlap syndrome (ACOS). This affects roughly 15–25% of those with COPD or asthma. Here, the fixed airway damage of COPD is combined with the reversible narrowing (spasms) typical of asthma, often triggered by things like cold air, pollen, exercise, or strong smells. This overlap can lead to more sudden worsenings, higher flare-up rates, and sometimes a faster drop in lung function. The positive side is that recognising ACOS can open up additional treatment options, such as inhalers that target both inflammation pathways more effectively. Alpha-1 Antitrypsin Deficiency-Related COPDIn a small number of cases (around 1–3% of all COPD), a rare inherited condition called alpha-1 antitrypsin deficiency is the main driver. The body doesn't produce enough of a protective protein (alpha-1 antitrypsin) that normally shields lung tissue from breakdown by the body's own enzymes. Without this protection, lung damage—usually emphysema—can develop much earlier in life, sometimes in your 30s or 40s, even with little or no smoking history. It can also affect the liver. A simple blood test can identify it, and if positive, there are specific treatments (like protein replacement infusions) alongside usual COPD care, plus important family screening. Understanding which type or combination you have helps your healthcare team choose the most suitable inhalers, breathing exercises, or further tests. The really encouraging part is that, regardless of the form, the same core actions—quitting smoking or irritants, getting vaccinated, starting medications early, and joining pulmonary rehabilitation—can make a big difference in slowing progression and giving you many more good days with fewer interruptions to the life you enjoy. 
Signs and Symptoms: What to Watch ForSpotting COPD early isn't always straightforward because symptoms often creep in gradually over years, and they're easy to dismiss as "just getting older," being out of shape, or even seasonal allergies. But learning to recognise these patterns can make a real difference—getting help sooner means better control of the condition and more chance to slow its progress. COPD symptoms tend to develop in stages, though not everyone experiences them in exactly the same way or at the same pace. The stages below give a general picture of how things can change over time. Early Stage SignsIn the beginning, symptoms are usually mild and come and go. They might not stop you from doing most things, but you'll start noticing small changes:
Many people put these down to age or lack of fitness, but if they keep happening or slowly get worse, it's worth mentioning to your GP. Middle Stage SymptomsAs COPD progresses, the effects become harder to ignore and start interfering with daily routines:
Flare-ups often need extra medication or sometimes a short course of antibiotics and steroids. Learning your personal warning signs helps you act quickly and avoid hospital visits. Late Stage SymptomsIn more advanced COPD, symptoms can become a major part of everyday life and affect almost everything you do:
At this stage, many people benefit from home oxygen therapy, stronger medications, and extra support services. Understanding Flare-Ups (Exacerbations)Flare-ups are sudden worsenings of symptoms that can feel frightening. Common triggers include chest infections (viral or bacterial), air pollution, cold weather, or even strong fumes. Signs to watch for:
Having a personal action plan from your GP or nurse—often including "rescue" medicines to start at home—can help you manage most flare-ups without needing emergency care. One important thing to remember: breathlessness that comes on suddenly or very severely, chest pain, confusion, or blue lips/fingers are emergency signs—call 999 straight away. COPD symptoms can vary day to day and season to season, but unlike normal ageing (where serious breathlessness is unusual), they tend to persist and slowly worsen without treatment. If any of this sounds familiar—for yourself or someone you care about—it's completely natural to feel concerned, but the NHS and organisations like Asthma + Lung UK emphasise that recognising symptoms early opens the door to effective treatments and support that can truly improve quality of life. You're taking a positive step just by reading and learning more. 
Causes and Risk FactorsNo one "deserves" COPD—it's usually the result of years of lung exposure to irritants, combined with factors that make some people more vulnerable. Understanding this can lift any sense of blame and show where positive changes can still make a big difference, even after symptoms start. The Role of SmokingThe main driver in the UK is long-term tobacco smoking, responsible for around 85-90% of cases according to NHS and other sources. The thousands of chemicals in cigarette smoke (and other tobacco products) directly inflame and damage the airway linings and air sacs over time, leading to the scarring and narrowing typical of COPD.
Quitting at any stage is the most powerful step you can take: it halts further damage immediately, often improves breathing within weeks, and significantly slows progression. Occupational and Environmental ExposuresBeyond smoking, breathing in harmful substances at work or in the environment plays a significant role, contributing to around 10-15% of cases in the UK (higher in some industries).
These irritants cause similar inflammation and scarring to smoking. If you've had such exposures, mention them to your GP—they're important for diagnosis and potential compensation claims. Other Risk FactorsSome factors are harder or impossible to change:
The Hopeful Side: What You Can InfluenceMany risks are modifiable, and acting on them protects lungs or slows COPD.
In 2026, with falling smoking rates and better awareness, more cases are preventable than ever. If you've never smoked but have symptoms, other factors could be at play—it's still worth checking. 
The Diagnosis Process: What Happens and Why It MattersReceiving a COPD diagnosis can bring mixed feelings—relief at finally having answers, alongside worries about the future—but it's a vital step that opens up personalised support and proven ways to manage the condition better. The process usually begins at your GP surgery:
The Key Test: SpirometryThe gold standard is post-bronchodilator spirometry—a straightforward breathing test recommended by NICE guidelines:
Quality-assured spirometry (often by trained nurses) is essential for accuracy. Additional Checks If Needed
Why bother? Early diagnosis means starting NICE-recommended treatments sooner—like optimised inhalers, pulmonary rehab, or smoking cessation—which can preserve lung function longer, reduce flare-ups by up to 20-30%, and improve daily life significantly. Many people delay, dismissing it as "just ageing," but acting early makes a real difference. Take someone with you if anxious, note symptoms in advance—the process empowers you with a clear plan ahead. 
Treatment and Management OptionsA COPD diagnosis might feel overwhelming at first, but the treatments available today—guided by NHS and NICE standards, along with international insights like the GOLD 2025 report—offer real ways to ease breathing, reduce flare-ups, boost energy, and help you get back to enjoying life more fully. There's no cure, but management has advanced significantly, and the approach is always personalised to your symptoms, lung function, flare-up history, and what suits you best. You'll have regular reviews (at least once a year, or more often if needed) to tweak things as your needs change. MedicationsMost medications come via inhalers, which deliver the drug straight to your lungs for quicker, safer effects with fewer side effects elsewhere in the body.
Getting your inhaler technique spot-on is key—poor technique means less medicine reaches your lungs. Ask your GP, nurse, or pharmacist for a check; spacers or different devices can make a huge difference, and many people notice big improvements after this. As of late 2025, exciting new options are emerging internationally (like ensifentrine, a nebulised treatment that relaxes airways and reduces inflammation, or dupilumab injections for those with type 2 inflammation and ongoing flare-ups). Availability on the NHS may follow further reviews, so discuss with your specialist if you have persistent symptoms. Non-Medication TherapiesThese often make the biggest difference to how you feel day-to-day and are strongly recommended alongside medicines.
Lifestyle and Self-Management StrategiesThese are essential and empower you to take control:
If you're supporting a loved one, gentle encouragement with inhalers, rehab attendance, or quitting attempts goes a long way—share the load to avoid burnout. With the right mix of these options, many people find COPD shifts from feeling all-consuming to something they manage well, freeing up energy for family, hobbies, and the things that matter most. Talk openly with your healthcare team—they're there to help find what works best for you. 
How to Live Well with COPD: Practical Tips and StrategiesLiving with COPD doesn't mean giving up the things you enjoy—it's about finding a new rhythm and making practical adjustments that help you stay in control. Many people discover that with the right strategies, symptoms become more manageable, energy levels improve, and life feels fuller again. Small changes often add up to big differences, and involving family or friends can make the journey feel less lonely. Mastering Breathing TechniquesWhen breathlessness hits, feeling panicky can make it worse. Learning simple techniques to breathe more efficiently can calm things down quickly and give you back a sense of control:
Practice these daily when you're feeling calm, so they become second nature. Asthma + Lung UK has free videos and downloadable guides that show exactly how to do them—highly recommended for getting started. Staying Active and Pacing Your DayIt might feel like the last thing you want to do, but keeping gently active is one of the best ways to build strength, improve mood, and actually reduce breathlessness over time:
Pulmonary rehabilitation programmes teach pacing perfectly, tailored to your level, and many people say it transforms how they feel about activity—from "I can't" to "I can do this in my own way." Eating Well and Staying NourishedBreathlessness can make eating feel exhausting, and some people lose or gain weight unintentionally—which affects energy and breathing:
Good nutrition supports your immune system too, helping fend off infections. Managing Emotional Wellbeing and RelationshipsCOPD can affect mood—feeling anxious about breathlessness, frustrated by limitations, or low because plans change. This is completely normal, and addressing it makes everything easier:
Intimacy can sometimes feel tricky with breathlessness, but pacing, different positions (e.g., side-lying), or using oxygen if prescribed can help—open conversation and NHS sexual health advice services support this too. Planning Ahead and Adapting Your HomeAs COPD progresses, simple adaptations keep independence longer:
Many people find that living with COPD brings unexpected positives: valuing time more, deepening relationships, and discovering new, gentler hobbies. You're not alone in this—support is there, and with these strategies, most days can still be good ones full of the people and activities you love. 
Myths and Facts About COPDMisunderstandings about COPD can add unnecessary worry, stigma, or delay in seeking help—so let's clear some of the most common ones with straightforward facts, based on trusted sources like the NHS, Asthma + Lung UK, and global guidelines. Myth: COPD is only a smoker's disease and somehow "deserved."Fact: While smoking causes the vast majority of cases, around 10-15% occur in non-smokers due to factors like long-term exposure to air pollution, workplace dust/fumes/chemicals, genetics (such as alpha-1 antitrypsin deficiency), or childhood respiratory issues. It's about lung irritation over time, not judgment—and support is available to everyone, regardless of history. Myth: Once you have COPD, nothing can slow it down—it's just constant worsening.Fact: Quitting smoking (or irritants) halts further damage straight away, often improving symptoms quickly. Modern treatments—like optimised inhalers, pulmonary rehabilitation, and self-management—can significantly ease breathlessness, reduce flare-ups, and preserve lung function for longer. Myth: Exercise is dangerous and will make COPD worse.Fact: Gentle, supervised activity (especially through pulmonary rehab) is one of the safest and most effective ways to build strength, improve endurance, and actually lessen day-to-day breathlessness over time. Myth: COPD is contagious, like a cold or flu.Fact: Absolutely not—COPD results from long-term lung damage, not from germs or viruses you can catch from someone else. Myth: Inhalers are addictive or damage your lungs further.Fact: Inhalers are safe, non-addictive tools that deliver medicine directly to your airways to open them up and reduce inflammation—no risk of addiction or additional harm when used as prescribed. Myth: COPD mainly affects older men.Fact: It now affects women just as much as men (due to changing smoking patterns over decades), 
Frequently Asked QuestionsCan COPD be cured completely?No, there's no full cure as the lung damage is permanent, but excellent management can control symptoms very well, slow progression dramatically, and allow many active, fulfilling years. How is COPD different from asthma?Asthma usually starts younger, with airway narrowing that's mostly reversible and triggered by allergens or exercise. COPD's obstruction comes from permanent damage and is largely fixed—though some people have an overlap (ACOS) needing treatments for both. Does quitting smoking help if symptoms are already there?Yes—it's the single most effective step, even after diagnosis. Your lungs begin repairing immediately, breathlessness often eases, flare-ups reduce, and further decline stops. What commonly triggers flare-ups?Respiratory infections (like colds or flu) are the top cause, along with cold air, pollution, dust, strong fumes, or smoke. Vaccinations, hand hygiene, avoiding triggers, and a personal action plan can greatly reduce them. Does what I eat affect COPD?Definitely—nutrient-rich, balanced foods support energy and immunity; smaller, frequent meals make eating less tiring when breathless; and staying hydrated helps thin mucus for easier clearance. Is pulmonary rehabilitation really effective?Yes, it's one of the best-supported treatments—most participants gain better stamina, fewer hospital visits, less breathlessness, and greater confidence in daily life. How can travel work with COPD?Many people travel successfully with planning: get a GP "fit-to-fly" letter, arrange portable oxygen if needed through your team, pack extra meds, pace activities, and choose destinations with good healthcare access. Does COPD strain the heart?It can, because the lungs work harder, putting extra pressure on the right side of the heart (leading to cor pulmonale in some cases). Regular check-ups catch this early, and treatments help protect heart health. Can you get COPD without smoking?Yes, about 10-15% of cases stem from occupational exposures, pollution, genetics, or other factors—always worth investigating symptoms, whatever your history. How does COPD impact closeness in relationships?Breathlessness can make physical intimacy more challenging, but adjustments like slower pacing, supportive positions, using oxygen if prescribed, or resting beforehand often help. Open conversations, and support from NHS counselling or specialist advice, make a big difference. What's new in COPD care as we head into 2026?Ongoing advances include smarter inhalers (some with apps to track use and technique), expanded access to pulmonary rehab, and emerging therapies like biologics (e.g., dupilumab for certain patients with type 2 inflammation) and novel inhalers (like ensifentrine). Research continues into targeted options—talk to your specialist about what's available or upcoming on the NHS. 
When to Seek Help and Key ResourcesKnowing when to get support is key to staying on top of COPD—if ongoing breathlessness, cough, or recurring flare-ups affect sleep, daily tasks, or enjoyment, see your GP soon. Acting early helps protect lung function and improves management. Urgent Signs – Call 999 or Go to A&E ImmediatelyDon't wait if you have:
Everyday Support and Reliable ResourcesYour GP or respiratory team coordinates ongoing care, including tests, reviews, and referrals. Keep a simple symptom diary to share at appointments—it really helps discussions. Trusted places for information and help:
Combining these often builds real confidence and connection. Save the numbers in your phone now—you're not alone, and reaching out can truly turn things around for the better. Important DisclaimerThis guide provides general information about chronic obstructive pulmonary disease (COPD) based on current UK knowledge and resources as of December 2025. It is not a substitute for professional medical advice, diagnosis, or treatment. If you or someone you know is experiencing symptoms of COPD, please consult a qualified healthcare professional as soon as possible. In a crisis or emergency, contact emergency services on 999 or a trusted helpline immediately. The information here is intended to inform and support, not to replace personalised care from doctors, specialists, or other qualified professionals.
© 2024 The Card Project Uk Ltd
VAT: 453 2087 06
|