Bio-degradable cards
Every card imaginable!
|
Bio-degradable cards Every card imaginable! What You Need To Know About Crohn's Disease
Understanding Crohn’s Disease: A Guide for Those Who Need AnswersWe know that finding out you have Crohn’s Disease, or even just suspecting you might, can feel overwhelming. There is so much information out there, and it can be hard to know what really matters when you are trying to make sense of it all. That is why we have put together this guide—to help you understand what Crohn’s Disease is, what the symptoms are, how it is diagnosed, and what life with the condition can look like. Whether you are newly diagnosed, waiting for answers, or supporting someone with Crohn’s, we want you to feel reassured that you are not alone. Many people are living full and happy lives with this condition, and while it does bring challenges, there is also a lot of support and understanding available. We have broken this article into sections that will hopefully answer your biggest questions and help you feel more in control. There is no right or wrong way to feel about a diagnosis like this, but knowing what to expect can make a huge difference. We are here to help, and we hope this guide gives you the information and reassurance you need.
Crohn’s Disease: More Than Just a Stomach AcheWhen people hear the words “Crohn’s Disease,” they often think of stomach pain and digestive issues, but there is so much more to it than that. If you or someone you love has recently been diagnosed, it can feel like stepping into an entirely new world of medical terms, doctor visits, and lifestyle changes. We understand how overwhelming that can be, and we are here to help. Crohn’s Disease is a lifelong condition that affects the digestive system, but it is not just about the gut. It is an autoimmune disease, which means the immune system mistakenly attacks the body’s own tissues, leading to inflammation. That inflammation can happen anywhere along the digestive tract, from the mouth to the rectum, and it does not stop there—it can also affect other parts of the body, leading to symptoms that people do not always expect. If you are trying to make sense of what it all means, you are not alone. Many people feel confused at first, but understanding the basics can make a huge difference. That is why we are going to walk you through what Crohn’s Disease really is, how it affects the body, and why it is so much more than just an upset stomach. What Exactly Is Crohn’s Disease?Crohn’s Disease is one of the two main types of inflammatory bowel disease (IBD), the other being ulcerative colitis. Unlike ulcerative colitis, which only affects the colon and rectum, Crohn’s Disease can appear anywhere in the digestive tract. It can also cause inflammation that spreads deep into the layers of the intestinal wall, making it more complicated to manage. Doctors and researchers still do not fully understand why some people develop Crohn’s Disease while others do not. What we do know is that it is not caused by eating the wrong foods, stress, or anything a person has done wrong. It is believed to be linked to a mix of genetic factors, immune system responses, and environmental triggers. Some people are diagnosed in childhood, while others do not get diagnosed until adulthood. The symptoms can range from mild to severe, and the condition itself can go through phases where it is active (a flare-up) or quiet (remission). The unpredictable nature of Crohn’s is one of the biggest challenges, but it is also why having the right information and support is so important. How Crohn’s Disease Affects the Digestive SystemCrohn’s Disease causes inflammation that can appear in patches anywhere along the digestive tract. Some people might only have inflammation in one small section of their intestines, while others may have it in multiple areas. Because of this, no two cases of Crohn’s look exactly the same. The most common areas affected include:
When the digestive tract is inflamed, it does not just cause pain. It can lead to long-term complications, including strictures (narrowed sections of the intestine), fistulas (abnormal connections between organs), and even blockages that require surgery. This is why managing inflammation early and keeping it under control is so important. Crohn’s Disease Affects More Than Just the GutOne of the things people do not always realise is that Crohn’s Disease does not just affect digestion—it can have an impact on the whole body. The immune system’s overactivity can cause symptoms far beyond the intestines, including:
These extraintestinal symptoms (symptoms outside the intestines) can be just as challenging as the digestive symptoms. They also highlight why Crohn’s Disease is about more than just stomach issues—it is a condition that can impact nearly every part of a person’s life. Who Gets Crohn’s Disease?Crohn’s Disease can affect anyone, but some groups are more likely to develop it than others. It is most commonly diagnosed in people between the ages of 15 and 35, though it can appear at any age. It is also more common in people with a family history of inflammatory bowel disease. Certain ethnic groups, particularly those of European descent and Jewish ancestry, have a higher risk of developing Crohn’s. However, the condition has been rising globally, and cases are increasing in areas where it was once rare. This suggests that environmental factors, such as diet, pollution, and gut bacteria imbalances, may play a role in triggering the disease. The Emotional Side of Crohn’s DiseaseGetting a Crohn’s diagnosis can bring a mix of emotions—relief at finally having an explanation, worry about what it means for the future, and frustration at the unpredictability of the condition. It is completely normal to feel a range of emotions, and it is important to know that support is available. Many people find comfort in connecting with others who have Crohn’s. Support groups, online communities, and even social media can be great places to find advice, share experiences, and feel understood. It can also help to have open conversations with family and friends so they understand what you are going through. Mental health is a big part of managing Crohn’s. Anxiety and depression are more common in people with chronic illnesses, and stress can sometimes trigger flare-ups. Finding ways to look after your mental well-being—whether it is through mindfulness, therapy, or hobbies that bring you joy—can make a big difference. Moving Forward with Crohn's Disease: Finding the Right InformationCrohn’s Disease is complex, but understanding how it works is the first step toward managing it. There is no cure, but there are treatments that can help control inflammation and improve quality of life. The more you learn, the more confident you will feel in making decisions about your health. In the next section, we will explore what researchers know about what causes Crohn’s Disease. There is no single answer, but looking at the latest science can help us understand why some people develop it while others do not. The Mystery of the Gut: What Causes Crohn’s Disease?One of the biggest questions people ask when they are diagnosed with Crohn’s Disease is, "Why me?" It is a natural reaction. When you are faced with a lifelong condition that brings so many challenges, it is only human to wonder how and why it happened. Unfortunately, Crohn’s Disease is still something of a medical mystery. Doctors and researchers have spent decades studying the causes, and while there is no single answer, we do know that Crohn’s is not random. It is linked to a combination of genetics, immune system reactions, environmental factors, and gut bacteria imbalances. Some people may be born with a higher risk, but something in their environment—like an infection, stress, or diet—might trigger it into action. Understanding what we do know about Crohn’s Disease can help people feel more in control. While we cannot yet pinpoint one exact cause, research is getting closer to uncovering the full picture. In this section, we will explore what the science tells us about why some people develop Crohn’s while others do not. Is Crohn’s Disease Genetic?If you have been diagnosed with Crohn’s, you might have wondered if it runs in families. The answer is yes—but it is not that simple. Studies show that Crohn’s Disease is more common in people with a family history of inflammatory bowel disease (IBD), which includes Crohn’s and ulcerative colitis. If you have a parent, sibling, or child with Crohn’s, your chances of developing it are higher than someone without a family history. In fact, around 15% of people with Crohn’s have a close relative with the condition. However, genetics alone do not explain everything. Scientists have identified over 200 different genes that may be linked to Crohn’s Disease, but having one of these genes does not mean you will definitely get it. Some people with the genes never develop Crohn’s, while others without any known genetic links do. This suggests that while genetics play a role, they are just one piece of the puzzle. Something else has to trigger the disease in people who are genetically predisposed. The Immune System Connection: When Defence Turns Into AttackCrohn’s Disease is an autoimmune condition, which means the immune system mistakenly attacks the body’s own tissues. Normally, the immune system protects us by fighting off harmful bacteria and viruses. But in people with Crohn’s, something goes wrong—immune cells start attacking the lining of the digestive tract, causing inflammation. But why does the immune system react this way? Researchers believe it could be linked to how the body responds to gut bacteria. Our digestive systems are full of bacteria, both good and bad, and they play a huge role in keeping us healthy. In people with Crohn’s, the immune system may mistakenly see certain gut bacteria as a threat and launch an attack. Studies have found that people with Crohn’s often have an imbalance in their gut microbiome—the community of bacteria, fungi, and other microorganisms that live in the intestines. Some researchers believe that in people who are genetically predisposed, an imbalance in gut bacteria could be the trigger that sets off the immune system’s overreaction. Environmental Triggers: Could Something Have Set It Off?If genetics and immune system dysfunction were the only causes of Crohn’s, we would expect the disease to be equally common everywhere in the world. But it is not. Crohn’s is far more common in some countries than others, which suggests that environmental factors must play a role. Research shows that Crohn’s Disease is most common in Western countries like the UK, the US, and Canada, and it has been on the rise in developing nations that have adopted a more Westernised lifestyle. This suggests that things like diet, hygiene, and pollution could be involved. Some of the environmental factors linked to Crohn’s Disease include:
The Role of Gut Bacteria: Is the Microbiome to Blame?The human gut is home to trillions of bacteria that help with digestion, immune function, and overall health. In recent years, scientists have discovered that people with Crohn’s Disease often have an imbalance in their gut microbiome. Some studies have found that people with Crohn’s have lower levels of certain beneficial bacteria and higher levels of harmful bacteria that can trigger inflammation. This imbalance might play a role in the immune system’s overreaction, leading to the chronic inflammation seen in Crohn’s Disease. This discovery has led to new research into treatments that focus on restoring balance in the gut. Some people with Crohn’s have found relief through probiotics, faecal microbiota transplants, and diets designed to promote healthy gut bacteria. While these are still being studied, they offer a promising glimpse into future treatments. Could Crohn’s Disease Be Prevented?Since we do not fully understand what causes Crohn’s, it is difficult to say whether it can be prevented. However, researchers are looking at ways to reduce the risk, particularly for people with a family history of the disease. Some possible ways to lower the risk of developing Crohn’s include:
While these steps are not guaranteed to prevent Crohn’s, they can help support overall gut health, which may reduce the risk. What We Still Do Not Know about Crohn's DiseaseDespite all the research, there are still many unanswered questions about Crohn’s Disease. Scientists are continuing to study the causes, and new discoveries are being made every year. Some of the biggest questions researchers are working on include:
As research progresses, we hope to have more answers. In the meantime, understanding the possible causes of Crohn’s can help people feel more informed about their condition. We will discuss this more in a later section though. In the next section, we will take a closer look at the symptoms of Crohn’s Disease—what they look like, how they vary from person to person, and what to do if you think you might have Crohn’s. 
Recognising the Warning Signs: Symptoms of Crohn’s Disease You Shouldn’t IgnoreCrohn’s Disease is known for being unpredictable. No two people experience it in exactly the same way, and symptoms can range from mild discomfort to severe pain and complications. Because it is a condition that affects the digestive system, many people assume that symptoms are limited to the gut, but Crohn’s can impact the whole body. One of the biggest challenges is that Crohn’s symptoms often come and go. Some people have long periods without symptoms (remission), while others experience frequent flare-ups. This unpredictability can make it difficult to know when something is a normal part of daily life and when it might be a sign of Crohn’s. Understanding the symptoms can help you or your loved one get the right diagnosis and treatment sooner. In this section, we will explore the most common signs of Crohn’s Disease, the lesser-known symptoms, and what to do if you suspect you may have it. Digestive Symptoms: More Than Just an Upset StomachSince Crohn’s Disease primarily affects the digestive tract, most people experience gastrointestinal symptoms. These can vary depending on which part of the intestines is affected, and they often come in waves, with flare-ups followed by periods of relief. Some of the most common digestive symptoms include:
These symptoms can appear gradually or come on suddenly. Some people go months or even years with mild symptoms before realising something is wrong, while others experience severe symptoms right away. Beyond the Gut: How Crohn’s Disease Affects the Rest of the BodyCrohn’s is not just a digestive condition—it is an autoimmune disease, which means it can affect multiple systems in the body. Many people are surprised to learn that symptoms can appear outside the intestines, sometimes even before gut symptoms begin. Some of the most common non-digestive symptoms include:
Because Crohn’s affects the immune system, it can cause widespread inflammation, leading to these symptoms. It is not uncommon for someone to visit a rheumatologist or dermatologist before they ever see a gastroenterologist. The Emotional and Mental Toll of Crohn’s DiseaseLiving with a chronic illness like Crohn’s can be emotionally draining. It is not just the physical symptoms that take a toll—there is also the stress of dealing with an unpredictable condition, managing medications, and adjusting to lifestyle changes. Some of the mental health challenges that come with Crohn’s include:
It is important to recognise that these feelings are valid, and seeking support from family, friends, or mental health professionals can make a big difference. Many people find comfort in joining support groups where they can talk to others who understand what they are going through. When to See a Doctor: Getting the Right DiagnosisBecause Crohn’s symptoms can mimic other digestive conditions like irritable bowel syndrome (IBS), food intolerances, or infections, it is not always easy to get a diagnosis. Many people go years without knowing they have Crohn’s, often being misdiagnosed along the way. You should see a doctor if you experience:
The sooner Crohn’s is diagnosed, the sooner treatment can begin. Early treatment can help prevent complications and improve quality of life. What Happens Next? Preparing for a DiagnosisIf you suspect Crohn’s, your doctor will likely start with blood tests, stool samples, and imaging tests like an MRI or CT scan. A colonoscopy is often needed to check for inflammation and take a biopsy. Getting a diagnosis can feel overwhelming, but knowing what to expect can help you feel more in control. The next section will cover the diagnostic process in more detail—what tests are used, what they look for, and how to prepare for them. Understanding how Crohn’s is diagnosed can help make the process less stressful and ensure you get the right care as soon as possible.
Getting the Answers You Deserve: How Crohn’s Disease Is DiagnosedWhen you have been dealing with unexplained symptoms for weeks, months, or even years, the thought of finally getting answers can bring both relief and anxiety. Many people with Crohn’s Disease go through a long journey before receiving a diagnosis, often facing misdiagnoses and frustration along the way. Because Crohn’s Disease shares symptoms with other conditions, doctors must rule out several possibilities before confirming the diagnosis. There is no single test that can say, "Yes, this is Crohn’s," which means the process can take time. But getting the right diagnosis is so important—it is the first step toward finding the best treatment and improving quality of life. If you or someone you love is preparing for medical tests, knowing what to expect can help make the process less overwhelming. In this section, we will walk through how Crohn’s is diagnosed, what tests doctors use, and what steps you can take to make sure you get the answers you need. The First Step: Talking to Your Doctor About SymptomsThe journey to a Crohn’s diagnosis usually starts with a conversation. Your doctor will ask about your symptoms, how long they have been happening, and whether they come and go or stay constant. It helps to keep a symptom diary before your appointment, noting things like:
This can give your doctor a clearer picture of what you are experiencing and help them decide what tests to run. Blood Tests: Looking for Clues in Your BodyOne of the first tests your doctor will order is a blood test. While blood tests alone cannot diagnose Crohn’s, they can show signs of inflammation, anaemia, or infection. Some key blood tests used in diagnosing Crohn’s include:
If blood tests suggest inflammation, your doctor will likely move on to further testing to find out what is causing it. Stool Tests: Checking for Inflammation and InfectionStool tests are another important tool in diagnosing Crohn’s. These tests can help rule out infections and check for signs of inflammation in the intestines. One of the most useful stool tests for Crohn’s is the faecal calprotectin test. This measures a protein that is released when there is inflammation in the gut. If calprotectin levels are high, it is a strong sign that something is going on in the intestines, and further testing is needed. Stool tests can also detect infections that might be causing symptoms, such as bacterial infections, parasites, or Clostridium difficile (C. diff), which can cause severe diarrhoea. Endoscopy and Colonoscopy: Taking a Closer LookIf blood and stool tests suggest Crohn’s, the next step is usually an endoscopy or colonoscopy. These tests allow doctors to see inside the digestive tract and check for inflammation, ulcers, or other signs of Crohn’s.
These tests can confirm whether there is inflammation, narrowing, or ulcers in the digestive tract, all of which are common in Crohn’s Disease. MRI and CT Scans: Imaging the Digestive TractIn some cases, doctors need a more detailed view of the intestines. This is where imaging tests like MRI and CT scans come in.
These scans help doctors see the extent of inflammation and any complications that might need treatment. Ruling Out Other ConditionsBecause Crohn’s Disease shares symptoms with other digestive disorders, doctors must rule out other possibilities before confirming a diagnosis. Some conditions that can mimic Crohn’s include:
Getting the right diagnosis is important because treatment for Crohn’s is different from these other conditions. How Long Does It Take to Get Diagnosed?Unfortunately, many people with Crohn’s Disease face delays in diagnosis. A study found that the average time from the first symptoms to a confirmed diagnosis is around three to five years. This is because symptoms can be mild at first, tests do not always give clear answers, and Crohn’s can be mistaken for other conditions. If you suspect Crohn’s and are struggling to get answers, do not give up. Keep pushing for further tests and seek a second opinion if needed. Early diagnosis can make a big difference in managing symptoms and preventing complications. What Happens After A Crohns Disease Diagnosis?Once Crohn’s Disease is confirmed, the next step is discussing treatment options. Treatment aims to reduce inflammation, control symptoms, and improve quality of life. This can include medications, lifestyle changes, and, in some cases, surgery. In the next section, we will explore what life with Crohn’s Disease looks like, including how to manage flare-ups, dietary changes, and ways to improve overall well-being while living with the condition. Navigating Life with Crohn’s Disease: Managing Symptoms and Finding ReliefA Crohn’s Disease diagnosis can feel overwhelming, but it does not have to define your life. Many people with Crohn’s go on to lead full and active lives, finding ways to manage symptoms, reduce flare-ups, and regain control over their health. The key is understanding your body, learning what works for you, and making adjustments that help keep symptoms in check. Crohn’s is a lifelong condition, and while there is no cure, there are many ways to manage it. Medications, diet, stress management, and lifestyle changes all play a role in keeping symptoms under control. In this section, we will explore how to manage flare-ups, prevent complications, and improve quality of life while living with Crohn’s. Understanding Flare-Ups: Why Symptoms Come and GoOne of the most frustrating things about Crohn’s Disease is its unpredictability. Symptoms can disappear for weeks or months, only to return suddenly and without warning. This is known as a flare-up, and it happens when inflammation in the digestive tract becomes active again. Flare-ups can be triggered by several factors, including:
Tracking symptoms and identifying personal triggers can help manage flare-ups more effectively. Medications for Crohn’s: Finding the Right TreatmentMedications are a key part of managing Crohn’s Disease. The goal is to reduce inflammation, control symptoms, and prevent complications. There are several types of medications used to treat Crohn’s, and treatment is often tailored to each person’s needs.
Finding the right medication can take time, and it often requires trial and error. Working closely with a doctor to adjust treatments as needed is important for long-term symptom control. The Role of Diet: What to Eat and What to AvoidFood does not cause Crohn’s Disease, but it can make symptoms better or worse. Every person is different, so finding the right diet can take time. Some people can eat almost anything, while others find certain foods trigger flare-ups. Common foods that may aggravate symptoms include:
During a flare-up, a low-residue diet may help by reducing the amount of undigested food passing through the intestines. This diet includes low-fibre foods like white rice, bananas, lean proteins, and well-cooked vegetables. Some people with Crohn’s find that an elemental diet (nutritionally complete liquid formulas) can help during severe flare-ups by giving the gut time to rest. It can be helpful to work with a dietitian to create a personalised eating plan that meets nutritional needs without worsening symptoms. Managing Stress and Mental Well-BeingLiving with a chronic illness like Crohn’s can be emotionally challenging. Stress does not cause Crohn’s, but it can make symptoms worse. Learning how to manage stress is an important part of symptom control. Some strategies that may help include:
Taking care of mental health is just as important as managing physical symptoms. Sleep and Fatigue: Managing Exhaustion with Crohn’sFatigue is one of the most common and frustrating symptoms of Crohn’s. It is not just feeling tired—it is an overwhelming exhaustion that does not go away with sleep. Some tips for managing fatigue include:
Getting good sleep is also important. Going to bed at the same time each night, limiting screen time before bed, and avoiding caffeine in the evening can help improve sleep quality. Preventing Complications: Keeping Crohn’s Under ControlCrohn’s Disease can lead to complications if it is not well managed. Some potential complications include:
Regular check-ups with a doctor, taking medications as prescribed, and making lifestyle adjustments can help prevent these complications. Staying Social: Travelling, Eating Out, and Living Life with Crohn’sA Crohn’s diagnosis does not mean giving up the things you love. With a little planning, it is possible to travel, eat out, and enjoy life while managing symptoms. Some tips for staying social with Crohn’s:
There are also practical tools that can help, like our Crohn’s Disease Medical ID Cards. These can be useful in situations where you need to quickly explain your condition, whether at work, while travelling, or in an emergency. Moving Forward: Living Well with Crohn’sWhile Crohn’s Disease is a lifelong condition, it does not have to control your life. With the right treatment, lifestyle adjustments, and support, many people manage their symptoms and continue doing the things they love. In the next section, we will explore how Crohn’s Disease affects the body beyond digestion, including joint pain, eye problems, and other complications that are often overlooked. Understanding the full impact of Crohn’s can help people get the right care and support for their needs. 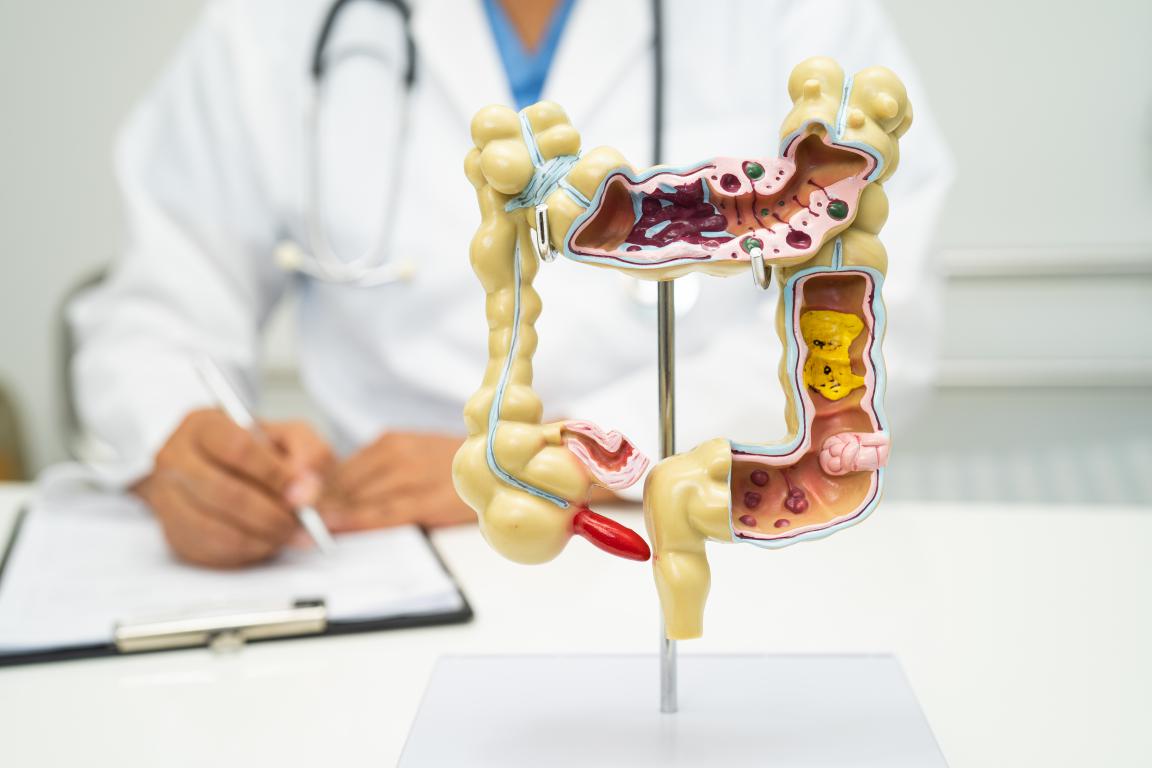
Crohn’s Disease Beyond Digestion: The Hidden Impact on the Rest of the BodyWhen we think of Crohn’s Disease, we often picture digestive issues—stomach pain, diarrhoea, and weight loss. But Crohn’s is much more than a gut condition. Because it is an autoimmune disease, it can affect the entire body, sometimes in ways that people do not expect. Many people with Crohn’s experience symptoms that have nothing to do with digestion. These can include joint pain, skin conditions, eye inflammation, and even mental health struggles. Some of these symptoms appear before Crohn’s is even diagnosed, which can make it harder to recognise the disease early. Understanding how Crohn’s affects the whole body can help people manage symptoms more effectively and get the right medical support. In this section, we will explore the complications that go beyond the gut and what can be done to manage them. Joint Pain and Arthritis: Why Do My Joints Hurt?One of the most common complications of Crohn’s Disease is joint pain. In fact, up to 30% of people with Crohn’s develop arthritis or joint inflammation at some point. This can happen for several reasons:
There are different types of joint issues that people with Crohn’s might experience:
Managing joint pain often involves anti-inflammatory medications, physical therapy, and regular exercise to keep the joints flexible. Some people find that swimming or yoga helps reduce stiffness and pain. Eye Inflammation: When Crohn’s Affects VisionMany people are surprised to learn that Crohn’s Disease can cause eye problems. Inflammation from Crohn’s can affect different parts of the eye, leading to pain, redness, and vision changes. The most common eye-related conditions include:
If eye symptoms appear, it is important to see an eye doctor (ophthalmologist) as soon as possible. Early treatment can prevent complications and protect vision. Skin Conditions: The Unexpected Link Between Crohn’s and the SkinThe skin is another area where Crohn’s Disease can cause unexpected symptoms. Some people notice rashes, ulcers, or painful lumps, especially during flare-ups. Some of the most common Crohn’s-related skin conditions include:
Many of these skin conditions improve once Crohn’s is under control. Topical creams, steroids, and immune-suppressing medications may also help manage symptoms. Fatigue: The Overwhelming Exhaustion That Comes with Crohn’sFatigue is one of the most frustrating symptoms of Crohn’s Disease. It is not just feeling tired—it is a deep, unshakable exhaustion that does not go away with rest. Many people with Crohn’s say that fatigue is one of the hardest parts of the disease to deal with. Several factors can contribute to Crohn’s-related fatigue:
Managing fatigue often requires a combination of approaches:
Understanding that fatigue is a real symptom—not just laziness—can help people feel more in control and get the support they need. Anaemia: The Hidden Cause of Weakness and DizzinessAnaemia is a common but often overlooked complication of Crohn’s Disease. It happens when the body does not have enough red blood cells to carry oxygen, leading to fatigue, dizziness, and shortness of breath. There are a few reasons why anaemia is so common in Crohn’s:
A simple blood test can check for anaemia, and treatment usually involves iron supplements, B12 injections, or dietary changes to increase iron intake. Mental Health and Crohn’s: The Emotional Toll of a Chronic IllnessLiving with a chronic illness can take a toll on mental health. Many people with Crohn’s experience anxiety, depression, or stress due to the unpredictability of symptoms. Some of the biggest mental health challenges include:
It is important to recognise that these feelings are normal, and seeking support can make a huge difference. Some helpful strategies include:
Taking care of mental health is just as important as managing physical symptoms. The Bigger Picture: Crohn’s as a Whole-Body DiseaseCrohn’s Disease is not just a digestive disorder—it is a condition that affects the whole body. Understanding the full range of symptoms can help people get the right care and prevent complications. In the next section, we will focus on practical ways to adjust to life with Crohn’s, from managing relationships to handling work and travel. Finding ways to live well with Crohn’s is possible, and we are here to help.
Thriving with Crohn’s: Adjusting to Life, Work, and Social SituationsA Crohn’s Disease diagnosis can change a lot of things, but it does not mean life has to stop. With the right adjustments, people with Crohn’s can continue to work, travel, eat out, and enjoy time with family and friends. While there are challenges, finding ways to navigate daily life can make a huge difference in feeling confident and in control. Crohn’s is unpredictable, and that can make planning ahead tricky. Some days, symptoms are manageable, and other days, they can feel overwhelming. Knowing how to prepare for different situations—whether it is a work meeting, a dinner with friends, or a long-haul flight—can help ease some of the stress. In this section, we will cover practical ways to adjust to life with Crohn’s, from handling relationships to managing work and travel. The goal is to find ways to live well with Crohn’s, rather than letting it take over. Talking About Crohn’s: How to Explain Your Condition to OthersOne of the hardest things about having Crohn’s Disease is explaining it to people who do not understand. It is not always obvious to others, and because symptoms like diarrhoea and fatigue are personal, many people avoid talking about it. But opening up—at least to close friends, family, or colleagues—can make life easier. People cannot support you if they do not know what you are going through. Some ways to make these conversations easier include:
Not everyone will “get it,” and that is okay. The important thing is surrounding yourself with people who are supportive and understanding. Working with Crohn’s: Balancing Health and CareerMany people with Crohn’s Disease continue to work successfully, but it can take some adjustments. Work environments vary, and some are more Crohn’s-friendly than others. Jobs with flexible schedules, remote work options, or understanding employers can make a huge difference. If Crohn’s symptoms interfere with work, some ways to manage include:
Some people find that self-employment or remote work gives them more flexibility. If traditional work is too challenging, exploring new career paths may be an option. Eating Out with Crohn’s: Enjoying Meals Without WorryDining out can be one of the most stressful parts of living with Crohn’s, especially when symptoms are unpredictable. But with a little planning, it is possible to eat out and still enjoy social events. Some ways to make eating out easier include:
Not every meal will go perfectly, and that is okay. Learning what works for you can make eating out feel less stressful over time. Travelling with Crohn’s: Tips for Stress-Free TripsWhether it is a weekend getaway or an international holiday, travelling with Crohn’s requires extra planning. The idea of being far from home can feel daunting, but with the right preparations, travelling is absolutely possible. Some key travel tips include:
Some people find that road trips or staying in accommodations with kitchens (like Airbnb) give them more control over their food and schedule. Relationships and Dating with Crohn’s: Navigating Personal ConnectionsCrohn’s Disease can sometimes feel like a barrier in relationships, whether with family, friends, or romantic partners. It is natural to worry about how others will react, but the right people will be understanding and supportive. Some ways to handle relationships with Crohn’s include:
Crohn’s does not have to limit relationships—it just means finding people who respect and support your journey. Finding Support: Connecting with Others Who UnderstandLiving with Crohn’s Disease can sometimes feel isolating, especially if those around you do not fully understand what you are going through. But you are not alone—there are many communities and resources available for support. Some ways to find support include:
Support can come from many places—family, friends, healthcare teams, or online communities. The important thing is knowing that help is available. Living Well with Crohn’s: Taking Control of Your HealthCrohn’s Disease brings challenges, but it does not have to define your life. With the right strategies, people with Crohn’s can work, travel, eat out, and maintain fulfilling relationships. Adjusting to life with Crohn’s takes time, and there will be ups and downs. But by planning ahead, listening to your body, and seeking support when needed, it is absolutely possible to live well with Crohn’s. In the next section, we will explore the latest treatments and future research into Crohn’s Disease. Understanding where science is headed can provide hope for better treatment options and improved quality of life. Hope for the Future: New Treatments and Research Advancing Crohn’s Disease CareFor many people living with Crohn’s Disease, the journey can feel like a never-ending cycle of medications, flare-ups, and adjustments. But there is hope. Medical research is advancing rapidly, with new treatments and potential breakthroughs that could transform the way Crohn’s is managed. While there is no cure yet, scientists and doctors are working hard to develop better ways to control symptoms, prevent complications, and improve quality of life. Understanding the latest developments in Crohn’s treatment can help people feel more in control of their condition. New medications, diet-based therapies, and even cutting-edge treatments like stem cell therapy and personalised medicine are showing promise. In this section, we will explore the current treatment options, the latest research, and what the future might hold for people living with Crohn’s Disease. The Changing Landscape of Crohn’s MedicationsFor years, Crohn’s Disease has been treated with a mix of anti-inflammatory drugs, immunosuppressants, steroids, and biologics. These treatments help reduce inflammation and manage symptoms, but they do not work for everyone, and some come with significant side effects. Researchers are now focusing on developing new medications that are more effective, have fewer side effects, and target Crohn’s at the source. Some of the latest advancements in Crohn’s medications include:
With more treatment options available, doctors are now able to personalise Crohn’s treatment plans based on individual needs, making it easier to find a medication that works. The Gut Microbiome: How Bacteria Could Hold the Key to New TreatmentsOne of the most exciting areas of Crohn’s research focuses on the gut microbiome—the trillions of bacteria that live in our intestines. Scientists have discovered that people with Crohn’s Disease often have an imbalance in their gut bacteria, with harmful bacteria thriving while beneficial bacteria are reduced. This imbalance may play a role in triggering inflammation and flare-ups. New therapies aimed at restoring gut health include:
By understanding the role of the microbiome, researchers hope to develop treatments that go beyond symptom management and address the root cause of Crohn’s. Stem Cell Therapy: Could This Be the Future of Crohn’s Treatment?One of the most promising new areas of Crohn’s research is stem cell therapy. This treatment involves using stem cells—cells that can develop into different types of tissues—to help repair damaged parts of the digestive tract and reset the immune system. Some potential uses of stem cell therapy for Crohn’s include:
While stem cell therapy is still in the experimental stages, it offers hope for people with severe Crohn’s who have not responded to other treatments. Can Diet and Nutrition Be a Treatment for Crohn’s?For years, doctors have debated the role of diet in Crohn’s Disease. While diet alone does not cause Crohn’s, research now shows that certain dietary changes can help manage symptoms and even promote healing in the gut. Some diet-based therapies that are being studied include:
Not every diet works for every person with Crohn’s, but understanding how food affects symptoms can be an important part of managing the disease. The Future of Crohn’s Treatment: What’s Next?Crohn’s Disease research is evolving quickly, and scientists are constantly looking for new ways to improve treatment. Some of the biggest areas of focus for future research include:
Finding Hope and Staying InformedThe future of Crohn’s Disease treatment is promising. With better medications, microbiome-based therapies, and new scientific advancements, people with Crohn’s have more options than ever before. While the disease is still unpredictable, research is moving in a direction that could make living with Crohn’s easier and, one day, even lead to a cure. Staying informed about new treatments can help people feel empowered in their Crohn’s journey. Talking to doctors about clinical trials, emerging therapies, and personalised treatment options can open doors to better care. In the final section, we will explore how to take control of Crohn’s Disease by building a strong support system, staying positive, and finding ways to live well despite the challenges. There is no one-size-fits-all approach, but with the right mindset and resources, people with Crohn’s can lead fulfilling lives. 
Living Beyond Crohn’s: Thriving, Not Just SurvivingA Crohn’s Disease diagnosis changes things, but it does not have to limit life. The journey with Crohn’s is different for everyone, but one thing remains true—life does not stop because of it. Finding ways to manage symptoms, build a support system, and maintain a positive mindset can help people with Crohn’s live fully, even on difficult days. This condition can feel overwhelming at times, but having the right knowledge and support makes all the difference. While there is no cure yet, people with Crohn’s are proving every day that they can achieve their goals, enjoy meaningful relationships, and take on life’s biggest moments. It all comes down to learning what works best for you and making adjustments that support your well-being. In this final section, we will explore ways to build confidence, find strength in support, and take control of Crohn’s instead of letting it take control of you. Building a Life You Love: Setting Goals with Crohn’sWhen dealing with a long-term health condition, it can be easy to focus on limitations. But shifting the mindset toward possibilities can open up new doors. Whether it is career ambitions, travel plans, or personal milestones, having Crohn’s does not mean giving up on goals. Some ways to set and achieve goals while managing Crohn’s include:
There is no “right” way to live with Crohn’s, and what works for one person may not work for another. The key is finding a balance that supports both health and happiness. Strength in Community: The Power of Connecting with OthersOne of the most powerful ways to navigate Crohn’s is by connecting with people who understand. The emotional side of chronic illness can be just as challenging as the physical symptoms, and having a support network makes a world of difference. Ways to find community and support include:
Having people to talk to—whether they are friends, family, or others with Crohn’s—can help make even the hardest days feel a little easier. Prioritising Well-Being: Mental Health, Rest, and Self-CareLiving with Crohn’s requires more than just medical treatment. Emotional well-being, self-care, and mental health are just as important. Stress, anxiety, and frustration can all impact symptoms, so finding ways to manage emotions is essential. Some strategies for prioritising mental health include:
Emotional resilience is built over time, and taking care of mental health is just as important as managing physical symptoms. Moving Forward with Confidence: Embracing Life with Crohn’sThere will always be ups and downs with Crohn’s, but that does not mean life has to be put on hold. With the right balance of medical care, lifestyle adjustments, and support, people with Crohn’s can continue to chase their dreams, build meaningful relationships, and experience joy in everyday moments. The journey with Crohn’s is unique for everyone, and there is no single path to managing it. The key is finding what works best for you, staying informed, and surrounding yourself with people who understand and support you. Life with Crohn’s is about more than just managing symptoms—it is about thriving in every way possible. With the right mindset, resources, and community, there is no limit to what can be achieved. Practical Support for Living with Crohn’s: How Our Medical ID Cards Can HelpWe hope this article has provided helpful information, reassurance, and support for anyone navigating life with Crohn’s Disease. Whether you are newly diagnosed or have been managing Crohn’s for years, having the right knowledge and resources can make a big difference. While the condition brings challenges, it is absolutely possible to live a full and rewarding life with the right tools and support. If you are looking for a practical way to make daily life easier, our Crohn’s Disease medical ID cards and awareness cards can help. These cards provide a simple and effective way to communicate your condition in different situations, whether you are dining out, travelling, at work, or in an emergency. Having a clear and discreet way to explain medical needs can remove stress and ensure you get the understanding and assistance you need. You can find our full range of Crohn’s Disease medical and awareness cards on our website at The Card Project UK. We are committed to providing useful and high-quality tools to help people living with Crohn’s feel more confident and prepared in everyday life. No matter where you are in your journey with Crohn’s, remember that you are not alone. There is support, understanding, and practical help available to make things easier. With the right mindset, resources, and people around you, Crohn’s does not have to define your life—you are in control of your own path forward. 
Essential UK Resources for Individuals Newly Diagnosed with Crohn's DiseaseReceiving a Crohn's Disease diagnosis can be overwhelming, but numerous UK-wide resources are available to provide support, information, and community connections. Here are some key organisations and platforms that can assist those newly diagnosed: Crohn's & Colitis UK is a leading charity dedicated to supporting individuals affected by Crohn's Disease and ulcerative colitis. They offer comprehensive information about the conditions, treatment options, and living with inflammatory bowel disease (IBD). Additionally, they provide access to support groups, educational events, and a helpline for personalised assistance. Guts UK focuses on the health of the digestive system and provides extensive resources on various gastrointestinal conditions, including Crohn's Disease. Their website features detailed information on symptoms, diagnosis, treatment options, and ongoing research. They also fund research projects aimed at improving the understanding and management of digestive diseases. NHS offers reliable and up-to-date information on Crohn's Disease, including symptoms, causes, diagnosis, treatment options, and advice on living with the condition. As the UK's publicly funded healthcare system, the NHS provides guidance on accessing medical care and support services across the country. The British Society of Gastroenterology (BSG) is a professional organisation for gastroenterologists in the UK. They offer patient resources, including guidelines and information on various gastrointestinal conditions like Crohn's Disease. Their materials can help patients understand the medical aspects of their condition and the standards of care they should expect. Healthtalk.org shares personal stories from individuals living with Crohn's Disease, providing insights into the experiences of others managing the condition. These narratives can offer comfort, practical advice, and a sense of community to those newly diagnosed. We know that dealing with Crohn’s Disease can feel like a lot, especially when you’re first diagnosed. But you don’t have to figure it all out on your own. These organisations are here to help, whether you need reliable information, advice from experts, or just to hear from others who understand what you’re going through. There’s a whole community out there ready to support you, and there’s always hope. Take things one step at a time, and remember—you are not alone in this. We’re here for you, and so are many others who truly understand.
© 2024 The Card Project Uk Ltd
VAT: 453 2087 06
|